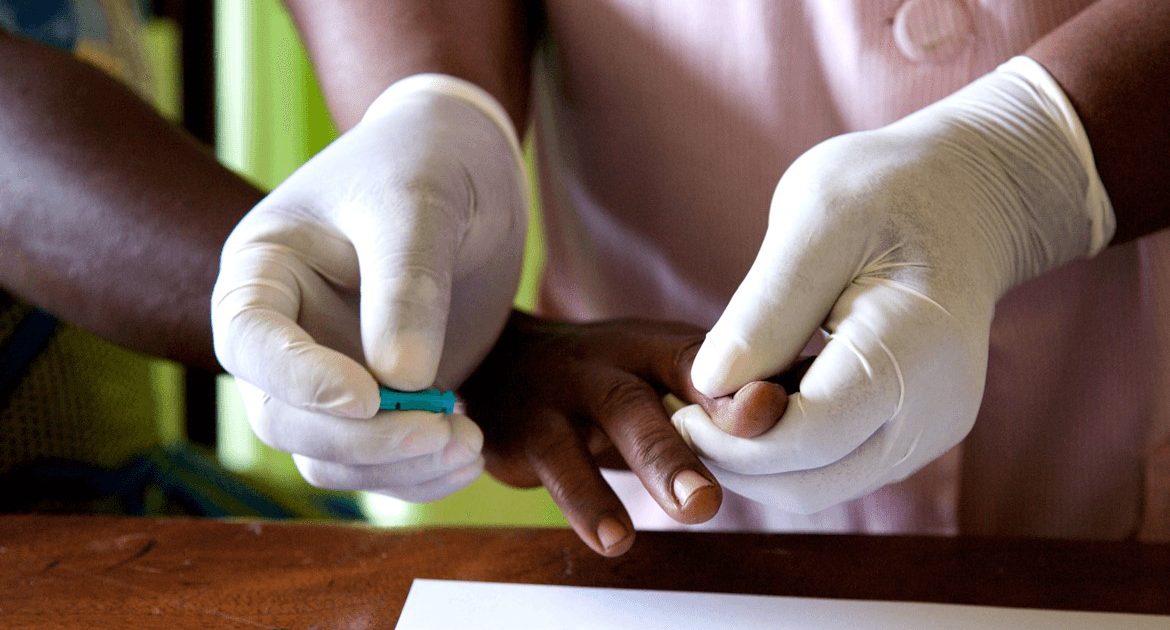
It is 10 am, Jane Wanjiku rummages through her bag in search of something that is visibly vital in her line of work. She pulls out a Bible, a bottle of mineral water and self-testing kits which she opens with enthusiasm.
Excitement lights up her face. She notes something in her pocket diary. Then she sighs, says she has been on demand lately. She has 15 homes to visit by evening. She has only 10 kits left. Five of her clients will have to wait until she gets more supplies. This could take time.
Wanjiku, a community health volunteer in a small and sleepy Tayari village of 57 homesteads in Molo says the HIV self-testing kit has been a wonder kit in her bid to ensure that people adopt it and constantly test and are aware of their HIV status. In Wanjiku`s own words, the uptake of the kits lately is encouraging. She attributes it to sustained awareness of the need for regular testing.
Community Health practitioners like Wanjiku are banking on self-driven initiatives in their campaign against HIV awareness and prevention in the effort of improving the campaign`s outcomes. This is against an unsettling backdrop of a spike in new HIV infections among teenagers in the Country. Nakuru is among counties that the ministry of Health has flagged as hotspots.
Adolescents are Wanjiku`s target. She wants them to regularly use the kits and her free counseling services in the bid to ensure a drop in new infections among a population that is considered most at risk.
Wanjiku who speaks with a glint in her eyes says the new infections among teenage girls from low income households in the area were triggered by the economic hardship that came in the wake of the novel coronavirus in 2020.
Having a considerable number of the adolescent girls from low income households where most of them are unable to afford sanitary pads, a majority of them resorted to indiscriminate sexual behavior in exchange for money to buy the pads and in some instances food.
Measures put in place to curb the spread of covid-19 such as lockdowns, closure of schools for a long period of time, curfew among other measures caused a diversion of health resources thus derailing their mission in down-scaling the numbers of new infections.
The health worker says that a considerable number of her clients privately request for the kit for fear of being stigmatized and discriminated against by those known to them. “Most of them fear their parents might perceive them in a negative way. Some of them request for the kits and counseling after having unprotected sex and attending parties,” she says adding, “I assure them of their confidentiality.”
Wanjiku only delivers the kits on request and the requests are made during her regular rounds in the village. Before using the kit, the user, in the company of a parent or guardian, undergoes counseling.
Then at their own comfort, blood or an oral sample fluid under the gum is collected, the HIV test is done and results interpreted in approximately 20 minutes. Once done, the kit is disposed of in a pit latrine.
However, Wanjiku notes that during the counseling session, a CHV advises the user of the kit to visit a health facility thereafter just for the result to be confirmed by a healthcare provider. This is because, the kit does not provide a definitive HIV-positive result.
Although the self-test kits that have an easy to read manual with diagrams are available in privately owned pharmacies, they retail at Sh500, which may prove prohibitive to underprivileged populations living in the slums.
Users in the informal settlements have called for free self-testing kits to expand access among the poor.
Wanjiku also attributes the increase of the new HIV infections among the adolescents in her community to drugs and substance abuse. She regrets that this has led to immorality and hampers the effort of CHVs in the fight against the HIV pandemic.
“Parents brewing illicit brews for example, make their female children vulnerable to abuse. In these chang’aa dens, the drunk customers prey on adolescent girls, impregnate them and most likely infect them with HIV,” she says.
The health worker adds, “in some instances, the children are also tempted to consume the brew, and when they get intoxicated, they misbehave and indulge in unprotected sex. Similar scenarios are also experienced in night parties where alcohol is always used.”
Wanjiku further discloses that the parents are a hindrance to the bid. She says some parents not only refuse to accompany their children but also dissuade them from using these kits.
“Some end up discovering their status when it is too late,” she notes.
For children living with HIV and the Orphans and Vulnerable Children (OVC), she says, they are registered and have programs that bring them together to share their experiences and also follow up on taking their ARVs.
Parents find it difficult to disclose to their children of their HIV status despite being well informed of the stages of disclosure; a training process they undergo before their child reaches the stage of full disclosure.
This group of children is said to have been on drugs all through their lives and when they reach the adolescent stage, many tend to resist taking their drugs, forcing the parents to devise means of informing them. To those who remain mum, the child becomes a threat to others until the day he or she finds out about his or her HIV status.
She advised parents to adhere to the stages of disclosure and send their children to counselors at the health facilities who will gladly attend to them and walk the journey with them thus ease the burden and help them accept their condition and take ARVs without fail.
Keeping clients’ information confidential on this matter, she says has kept her going and she has earned the trust of many who have confidence in her work.
A clinician co-coordinating HIV and Sexually Transmitted Infection (STI) in Molo sub-county, Nancy Keiyo alludes to the fact that the kits have been fully integrated into the community through the help of the CHV.
Nakuru County has got an estimated 65, 860 people living with HIV as per the 2019 national HIV study of whom 44,000 have been identified through testing and are on ARVs. In the same period there were 578 new HIV infections among the adolescents out of the 1,765 identified within the County. Health officials’ term this as highest compared to other key populations including sex workers, gay men, and transgender among others.
Nakuru County Aids and STI Coordinator (CASCO) Rachael Kyuna noted that they are committed to a scaled up health education within communities using the CHVs as contact persons.
Public Health workers empower the CHV with up to date and easy to use information, data collection and data knowledge, skills that Kyuna says, enable CHVs to play key roles in disseminating the information to communities.
She continues to say that at the sub-county level, there are health promotion experts who normally package the information on preventive measures and pass it through to various available media channels and besides make visits to learning institutions with intelligible messages about prevention and control of HIV.
Once a person uses the self-test kit that is allowed for use by 15 year olds and above and gets a positive result, Kyuna notes, the client is supposed to visit a health facility where the test will be conducted thrice before confirmation by different trained personnel. This is all in a bid to give precise results.
In as much as there is health education promotion of the self-test kit, Kyuna insists that people should visit the hospital to ascertain the results. She advocated use of the kits among the adolescents who are sexually active adding that there is need to clearly follow instructions for use.
Recent data has indicated that 98 per cent of new HIV infections occur every week among the adolescents, 21 per cent of Ante-Natal Clinic (ANC) attendants of the similar age group and 53 per cent of Sexually Gender Based Violence (SGBV).
Additionally, the research finding indicates that adolescents contribute to 61 per cent of all new adult HIV infections nationally.
In Nakuru County, Kyuna points out, only 16 per cent of the young mothers attend ANC down from 18 per cent in 2018 yet this age group remains sexually active.
The devolved unit is therefore reaching out to schools, talking to teachers to ensure that students get the appropriate information focusing on Abstinence, Be aware of oneself and Care for oneself and others, (ABC) that will empower them in the fight against HIV AIDS.
Kyuna further appeals to parents, religious leaders and teachers to sustain the campaign at their various levels to help curb the scourge. Additionally, she urged members of the community not to take advantage of adolescents under their care but instead be role models to the adolescents.
Wanjiku hopes the stakeholder driven campaign will continue and vowed to continue with her idea of testing and counseling for a healthy community.
By Emily Kadzo